Potential Risks to Skipping Breakfast

Potential Risks to Skipping Breakfast
Many people know the saying, “Breakfast is the most important meal of the day” yet fasting until noon (one type of intermittent fasting) has become popular and mainstream. While it may be beneficial for some, Stanford Lifestyle Medicine physicians and researchers caution new fasters and want to highlight some important considerations for those thinking about skipping breakfast.
“Limiting the time frame that calories are consumed has become a popular dietary strategy to improve health and aid in weight management. Fasting until noon is one of these popular strategies,” says Jonathan Bonnet, MD, MPH Stanford Lifestyle Medicine Physician. “For some, this may work well, however, the preponderance of evidence suggests that weight loss is modest and no more beneficial than overall caloric restriction.”
Side Effects of Skipping Breakfast
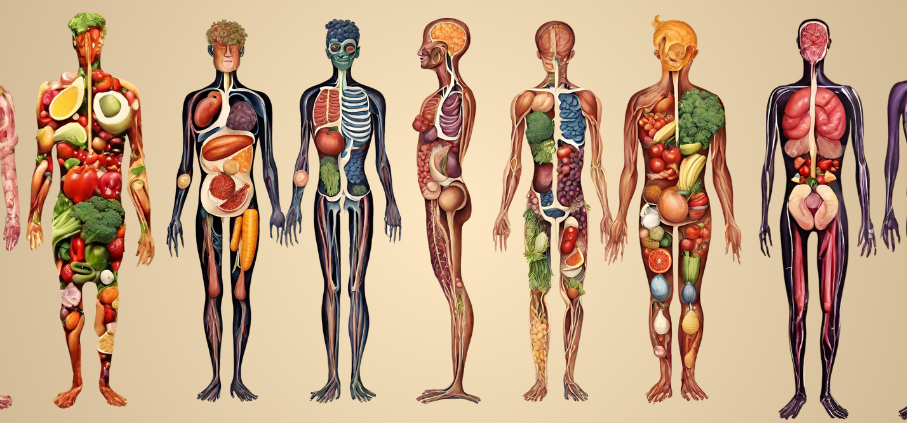
Delaying the first meal of the day until noon falls into the category of time-restricted eating. Although this eating pattern may help someone reduce their overall caloric intake, it may also lead to disruptive changes to their circadian rhythm, which could negatively affect sleep, as well as insulin sensitivity and glucose uptake.
In a recent review, researchers discussed the potential impacts of skipping morning-time breakfast. The review reported associations between skipping breakfast and an increased risk of developing obesity or type 2 diabetes. These studies primarily focused on the short-term effects of introducing the morning fasting behavior into one’s routine, however, the long-term effects of habitually fasting until noon are still being studied.
Feeding the Circadian Rhythm
Eating breakfast early in the morning is one signal that influences the genetic pathways underlying the circadian oscillations in the gut, which are critical for predicting daily energy levels and jump-starting metabolism. Thus, skipping breakfast could weaken the signaling of these clock genes and could be one reason why some people that fast until noon experience higher hunger levels throughout the day.
“Skipping breakfast impacts numerous circadian signals within the body that may be suboptimal,” says Dr. Bonnet. “If someone wanted to try a time-restricted approach, they may experience more benefits from having an earlier eating window (to include a more substantial breakfast) with limited late-night food consumption.”
While research is still trying to understand how impactful these circadian changes are long-term, it is possible that irregular or inadequate fueling of the body may negatively affect one’s body weight, glucose metabolism, and overall health. Thus, it may be more beneficial for one’s health to prioritize consistently eating meals at the same time every day.
“From a circadian perspective, regularity is key,” says Jamie Zeitzer, PhD, Stanford University Professor and member of the Stanford Lifestyle Medicine Sleep team. “The circadian system anticipates signals, like food intake, at certain times of the day and synchronizes gut activity in response.”
Not All Fasting is Bad
Fasting until noon is just one type of eating pattern and not all types of fasting have negative health effects. There are other forms of intermittent fasting that are currently being studied in longevity science due to their ability to build resilience to stress and diseases. For individuals facing obesity and related chronic diseases, time-restricted eating approaches (that maintain the morning fasting window), have not been shown to be significantly more beneficial for weight loss than those following overall caloric restriction methods.
“For those with weight-related cardiometabolic conditions like Type 2 Diabetes, most forms of weight loss can improve their condition,” says Dr. Bonnet. “Finding a way to create a sustainable caloric deficit to lose weight is a challenge, so if some variant of intermittent fasting works for them, it may be the key to start improving their overall health.”
Anyone considering any form of intermittent fasting or time-restricted eating should consult with their physician to make sure that it is the healthiest decision for them both physically and mentally.