The Impact of the Western Diet on Diverticulitis
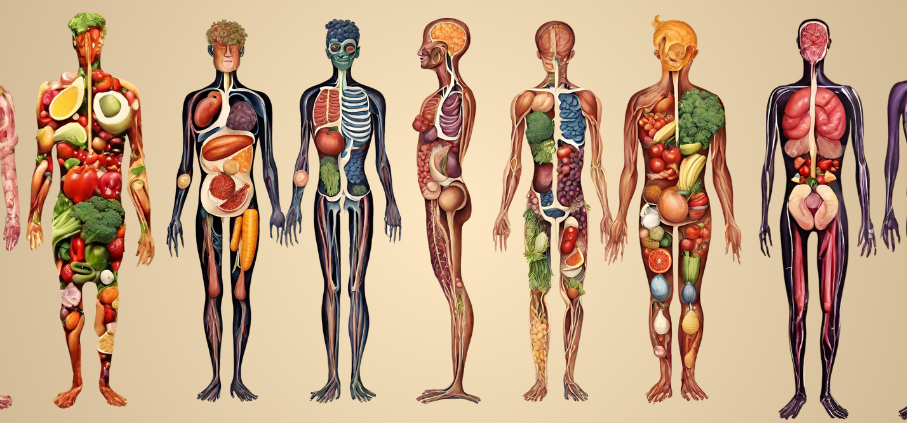
Recognizing the vital connection between colorectal health and diet has never been more important, given the escalating prevalence of colorectal diseases in Western societies. According to Cindy Kin, MD, MS, a colorectal surgeon at Stanford, many of these conditions are preventable and are linked to the dietary patterns we develop early in life.
“Many people in the US have a chronically low fiber diet high in inflammatory foods beginning in childhood that leads to microbiome dysbiosis, as well as actual structural changes to the gastrointestinal tract,” says Dr. Kin. “Over time, this leads to numerous colorectal diseases, some of which are irreversible and require surgery.”
One specific condition that has seen a significant increase in prevalence in the last 50 years is diverticulosis, characterized by the formation of irreversible outpouchings in the colon. This condition affects approximately one in three individuals aged 50-59 and virtually everyone over the age of 90 in the US.
Diverticulosis itself does not cause symptoms, and most patients only find out about them when they have a colonoscopy. However, anyone with these diverticular outpouchings is at risk of developing diverticulitis, a painful disease triggered by perforations in one or more diverticula. Diverticulitis may range in severity from mild to severe and life-threatening, depending on the size of the perforation. A tiny pinhole perforation that seals itself quickly might cause a little pain and inflammation that can be treated with oral antibiotics. On the other end of the spectrum, a larger perforation that leaks air and stool into the surrounding abdominal cavity can make someone so sick that they would need to have emergency surgery.
“Three to five million people get some sort of treatment for diverticulitis per year in the US,” says Dr. Kin, “A proportion of those people need surgery, making diverticulitis one of the most common reasons for colon surgery.”
The Growing Prevalence of Diverticulitis in the US
Diverticulosis became a known problem in the US in the early 1900s, coinciding with major technological advancements, such as fertilizers, preservatives, and factory farming. These advancements caused significant changes in the American diet. Regular consumption of high-fiber, farm-fresh whole foods was replaced by processed foods lacking in essential nutrients. Diets also became increasingly saturated with meats, fats, and sugars, replacing fruits, vegetables, and whole grains. As our diets followed this trend and became more “Westernized,” cases of diverticulitis significantly increased.
This US-specific increase in diverticulitis is in stark contrast to the nearly negligible incidence found in regions of the world where diets are rich in fiber. In Asian countries, where the diet is becoming more influenced by Western culture, we observe a rising incidence of diverticulitis in the last 30 years. “Diverticulitis is almost entirely a disease of our Westernized diet, low in fiber and high in ultra-processed foods and saturated fat,” says Dr. Kin.
What to Eat (and Not to Eat) to Reduce the Risk of Diverticulitis
c
Fiber
Dietary fiber, found in various forms in vegetables, legumes, and whole grains play a critical role in maintaining soft, easily eliminable stool. Conversely, diets lacking in fiber often lead to hard smaller-caliber stools and constipation, prompting the colon to work extra hard to move it through. Years of sustained high pressure within the colon is thought to be the root cause of diverticulosis, the presence of outpouchings in the wall of the colon. These outpouchings, or diverticula, form as the colon is squeezing so hard that it pushes out a portion of its own wall. The diverticula are weaker than the rest of the colon wall, and are more prone to bleeding and perforations. Research has consistently demonstrated that diets rich in fiber are strongly associated with a reduced risk of developing diverticular disease.
For many years, the widespread recommendation for those with diverticular disease was to avoid nuts, seeds, and popcorn due to the perceived risk of these foods getting trapped in the diverticular outpouchings. However, research suggests this is not the case and eating these foods may actually reduce one’s risk of developing diverticular disease due to their fiber content. “In all my years operating on diverticulitis, I have never seen a popcorn kernel or a sunflower seed poking out of a diverticulum causing a perforation, yet patients continue to steer clear of these fiber-rich foods due to this persistent diet myth,” says Dr. Kin.
Dr. Kin’s recommended daily fiber intake for women is 30-35 grams and 35-40 grams for men. While there are numerous fiber supplements available to help reach this daily goal, Dr. Kin recommends getting your fiber from dietary sources because foods that naturally contain fiber offer a multitude of advantages that extend beyond digestive health, such as lowering cholesterol and weight management to lower the risk of heart disease, stroke, diabetes, and other chronic diseases.
“If your body is not used to a high-fiber diet, gradually add fiber into your daily meals to allow your body to adjust over a couple weeks,” cautions Dr. Kin. “For most people, the gassiness that can happen with eating more fiber will get better pretty quickly, so don’t give up! A little gas upfront for a lifetime of colon health is a small price to pay.”
Processed Foods
Processed foods often lack the essential dietary fiber that whole unprocessed foods naturally provide. Additionally, the overconsumption of refined sugars and saturated fats in processed foods has been associated with several adverse health effects, including changes in gut microbiota composition and an increased risk of inflammation within the gastrointestinal tract. These factors can further exacerbate the risk of diverticular disease development.
Red Meats
Diets high in red meat are linked to diverticulitis, with a large-scale study finding the risk increasing by 18 percent for every additional serving of processed red meat. Red meat is associated with inflammation within several internal organs, and excessive consumption over time has numerous health consequences, including deteriorating colorectal health.
To prevent diverticulitis and several other colorectal diseases, Dr. Kin highly recommends “adopting a whole food, plant-based diet for its exceptional combination of high fiber content and nutrient-dense antioxidant properties.”