The Role of Physical Activity in Successful Aging
Physical activity is considered of utmost importance in the field of research on successful aging. However, the question of what physical activity should look like throughout one’s lifetime remains. While walking is an excellent way to begin exercising, it may not be sufficient for healthy aging in the long run. Instead, research suggests incorporating a variety of exercise modalities into your routine to improve overall health and well-being throughout life. Resistance training – which involves weights, resistance bands, and body weight exercise – plays an important role in muscle and bone density, as well as in cardiovascular health (more on page 4). The value of proprioception in physical activity is also emphasized. Proprioception is the body’s ability to orient and sense its own movement and is important for safe and efficient movement throughout life.
Balance exercises improve the mind-muscle connection and can help to prevent falls. These exercises include Tai Chi and Yoga, which are low-intensity physical activities that increase cerebral blood flow and involve sustained attention. Furthermore, endurance exercises, such as running or swimming, reduce inflammation, improve cardiovascular health, and can result in healthy gut microbiomes (Clauss et al. 2021 and Estaki et al. 2016) (more on page 4). Members of the Stanford Lifestyle Team are currently researching the role of physical activity in successful aging. To learn more about an ongoing physical activity intervention trial for cardiovascular disease prevention keep on reading!
Key Guidelines for Older Adults
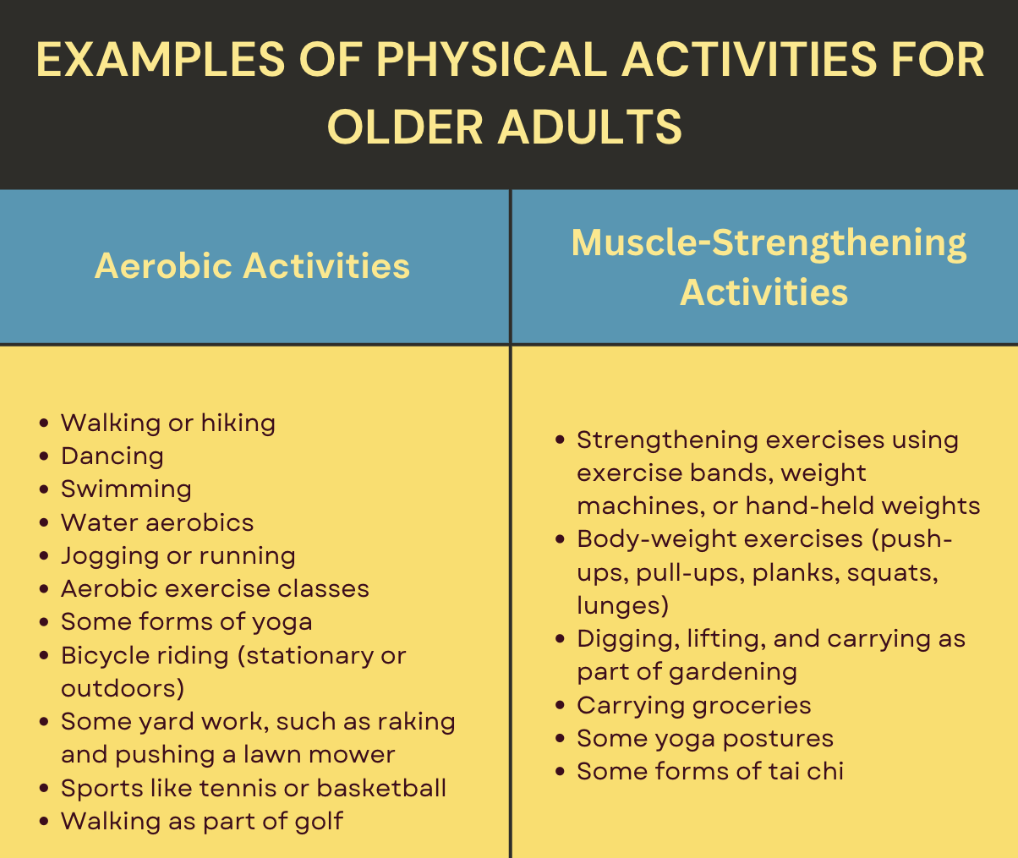
For substantial health benefits, adults should at least do either: 150 minutes to 300 minutes a week of moderate-intensity physical activity 75 minutes to 150 minutes a week of vigorous-intensity aerobic physical activity or an equivalent combination of moderate- and vigorous-intensity aerobic activity. With aerobic activity preferably spread throughout the week
Additional health benefits are gained by engaging in physical activity beyond these hours. Adults should also do muscle-strengthening and balance activities on 2 or more days a week.
- Balance activities can improve the ability to resist forces within or outside of the body that causes falls.
- Balance training examples include walking heel-to-toe, practicing standing from a sitting position, and using a wobble board. Strengthening muscles of the back, abdomen, and legs also improves balance.
MORE TO COME ON PHYSICAL ACTIVITY FOR HEALTHY AGING IN FUTURE NEWSLETTERS
Introducing Our Team’s Research
Women’s Health Initiative Strong and Healthy (WHISH): A pragmatic physical activity intervention trial for cardiovascular disease prevention

While national guidelines promote physical activity to prevent cardiovascular disease (CVD), the Women’s Health Initiative Strong and Healthy (WHISH) study is the first randomized control trial to test the effectiveness of increasing physical activity for cardiovascular prevention in older women. The WHISH trial is unique in its scale and study design. 49,333 women aged 68 to 99 were randomly assigned to two groups. While one group received a physical activity program, the other group continued with their usual activities. After 8 years of follow-up, the study aims to compare the heart health of these two groups. For the group that was assigned to the intervention, a multi-component physical activity intervention is being delivered.
Based on intervention goals from the U.S. Department of Health and Human Services, the physical activity program in WHISH aims to increase or maintain aerobic physical activity (primarily walking), decrease sedentary behavior (especially sitting), and increase multicomponent physical activity regarding muscle-strengthening, balance, and flexibility. The intervention is delivered through multiple channels including quarterly (seasonal) WHISHful Actions newsletters, with inserts targeted at 3 participant groups based on lower, middle and higher levels of self-reported physical functioning and physical activity levels, monthly telephone calls and emails with motivational messages, and access to exercise resources on the WHISH website. Crucial to our understanding of CVD prevention in older women, the comprehensive and pragmatic approach of the WHISH study make it a landmark study that will inform policy and future research.
Learn more about the WHISH study here: https://whish.stanford.edu/about/

Dr. Marcia L. Stefanick
Movement & Exercise Pillar of Stanford Lifestyle Medicine
Dr. Stefanick is a Professor of Medicine, Professor of Obstetrics and Gynecology, and a member of the Lifestyle Medicine Program at Stanford University. Her research focuses on chronic disease prevention in men and women. She is the Principal Investigator of the Women’s Health Initiative Strong and Healthy (WHISH), a large-scale physical activity intervention trial investigating whether moving more and sitting less can reduce risk of heart disease in older women.
Program Updates
NEW MEMBERS OF THE LIFESTYLE MEDICINE TEAM
Anne Friedlander, PhD Adjunct Professor of Human Biology and Exercise Physiologist, Stanford University
Emily Kraus, MD Clinical Assistant Professor of Orthopaedic Surgery, Stanford Children’s Orthopedic and Sports Medicine Center
Marcia Stefanick, PhD Professor of Medicine, Obstetrics and Gynecology, Stanford Prevention Research Center
Stacy Sims, PhD, MSc, SIMS Exercise Physiologist and Nutrition Scientist Senior Research Associate, Auckland University of Technology
Michelle Hauser, MD, MS, MPA, FACLM, Chef Clinical Associate Professor of Medicine, Stanford University
Cheri Mah, MD, MS Head, Sleep Medicine at UCSF School of Medicine
Jamie Zeitzer, PhD Professor of Psychiatry & Behavioral Sciences Sleep Medicine, Stanford University
Rafael Pelayo, MD Clinical Professor, Psychiatry and Behavioral Sciences Sleep Medicine, Stanford University
Corey Rovzar, PhD, DPT Postdoctoral Fellow Prevention Research Center Stanford School of Medicine
Sean Spencer, MD, PhD Gastroenterologist and Physician Scientist, Stanford University
Alia Crum, PhD Associate Professor of Psychology Instructor of Medicine, Primary Care & Population Health
SEED GRANT UPDATES
Effect of Meal Timing Modifications on Glucose Metabolism and Sleep In Individuals At Risk For Type 2 Diabetes
PI: Heyjun Park, PhD
Diet is a core lifestyle behavior that can be modified to prevent and manage type 2 diabetes (T2D). Food is a signal that synchronizes the circadian clock system, which controls thousands of metabolic processes. Therefore, the timing of meals can affect glucose metabolism. Our central hypothesis is that optimizing meal timing will confer glycemic control benefits, shift microbiome profiles in a positive direction, and improve sleep among people with prediabetes and T2D. To address this research question, our study will examine the impact of different meal timing modifications on glucose metabolism, gut microbiome, and sleep in individuals with prediabetes and T2D through a 12-week randomized controlled crossover design. Specifically, we will investigate the timing of the dominant daily energy load, the time of meals relative to sleep, and the timing of the energy intake window. The study has recently been launched and is currently enrolling participants.




![newsletter 1.1[4] NEWSLETTER](https://longevity.stanford.edu/lifestyle/wp-content/uploads/sites/31/2022/04/newsletter-1.14.png)